Pathology experts review challenges and opportunities in treatment selection for muscle-invasive bladder cancer (MIBC), propose traditional pathology method to achieve same results as molecular profiling at lower cost
Research has shown that some types of bladder cancer respond well to treatment and other types are resistant, yet molecular subtyping, which can help better define a patient’s cancer and direct them to a more targeted treatment, is not performed in the clinic. This means that patients are often treated with a one-size-fits-all approach. Despite recent research progress, the movement of MIBC subtyping to the clinic has stagnated.
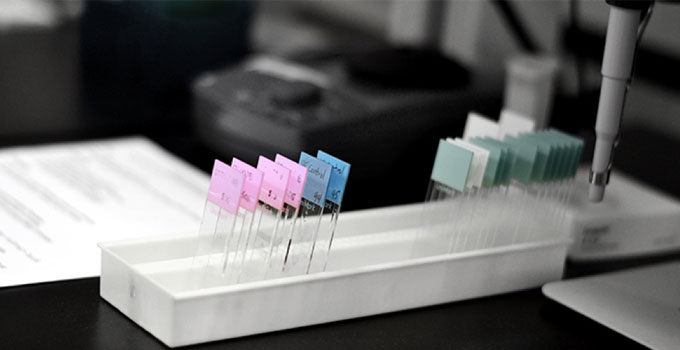
A group of expert pathologists recently reviewed opportunities for MIBC subtyping and the challenges facing its adoption. Their analysis found that a simple technique using immunohistochemistry (IHC), a traditional antibody-based pathology method, could serve as a faster and less expensive alternative to sequencing, while achieving the same patient selection outcomes to guide therapy.
“We envision a world where subtyping is efficiently and effectively deployed to ensure that patients who will benefit from treatment get the treatment they need, while others who may gain no benefit from treatment are spared the associated negative side effects,” says Dr. David Berman, Director of the Queen’s Cancer Research Institute and senior author of the review.
Since IHC is commonplace in clinical labs, subtyping MIBC in this way could be easily integrated into practice, meaning nearly all hospitals could perform these tests effectively, quickly and inexpensively. Instead of looking across tens of thousands of genes, which may cost thousands of dollars, the IHC algorithm could use three immunostains to gain valuable information about a patient’s cancer for a few hundred dollars. The authors also suggest that IHC-based subtyping is a simple way to overcome the challenge of the complex mixture of cells within bladder cancer tissue samples that often cloud sequencing analysis.
“Genome and transcriptome sequencing has been crucial to our understanding of MIBC, but the translation of this understanding to the clinic could be accelerated by using simpler assays,” says Dr. John Bartlett, Program Director of Diagnostic Development at OICR and co-author of the paper. “By using established diagnostic assays to distinguish relevant molecular subtypes, research discoveries about these subtypes can be used to rapidly to inform treatment selection in the clinic.”
“The potential efficiency of an IHC-based technique in MIBC subtyping is clear,” says Berman. “We look forward to developing and furthering an algorithm to bring MIBC subtyping into practice.”
