By combining new knowledge from the fields of stem cell biology and genetics, a group of Ontario researchers led by Dr. John Dick have solved the mystery of why some acute myeloid leukemia (AML) patients relapse after initial treatment.
They have traced the origins of AML relapse to rare therapy-resistant leukemia stem cells that are already present at diagnosis – before chemotherapy even begins. They have also identified two distinct stem cell like populations from which relapse can arise in different patients.
These findings can help to identify at an earlier stage patients who will relapse and to find better, more targeted therapeutic approaches to AML.
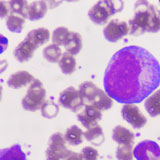
AML is an aggressive form of cancer that starts in the blood stem cells in the bone marrow. It is the most common type of leukemia in adults, with 1,315 Canadians diagnosed each year. Long-term survival remains low because most patients relapse despite going into remission after initial treatment.
In order to find out why some patients relapse and some don’t, Dr. Dick’s team brought together knowledge from cancer stem cell biology and genetics. They analyzed and compared two types of sample from each patient: one sample of blood taken at the initial clinical visit and one sample taken after treatment when the disease recurred.
“First, we asked what are the similarities and differences between these samples. We carried out detailed genetic studies and used whole genome sequencing to look at every part of the DNA at diagnosis, and every part of the DNA at relapse,” said Dick. “Next, we asked in which cells are genetic changes occurring.”
He noted that the breakthrough was possible because of the evolution of deep sequencing technology. The cutting-edge technology allowed them to take a new approach to work they’ve been doing for decades.
The findings, which were published in the prestigious journal Nature, also builds on recent research from Dick’s team that details the development of a “stemness biomarker” – a 17-gene signature derived from leukemia stem cells that can predict at diagnosis which AML patients will respond to standard treatment.
“Our new findings add to that knowledge and we hope that we will soon have a new biomarker that will tell whether a patient will respond to standard chemotherapy, and then another to track patients in remission to identify those where treatment failed and the rare leukemia stem cells are coming back,” said Dick.
“These new kinds of biomarkers will lead to new kinds of clinical trials with targeted chemotherapy. Right now, everybody gets one-size-fits-all because in AML we’ve never had any opportunity to identify patients upfront, only after they relapse. Now we have the first step to identify these patients at the outset and during remission.”
Dick is a Senior Scientist at Princess Margaret Cancer Centre, University Health Network and Co-leader of OICR’s Acute Leukemia Translational Research Initiative. This study was primarily undertaken by postdoctoral fellow Dr. Liran Shlush and Scientific Associate Dr. Amanda Mitchell at University Health Network.
The research was funded by the Ontario Institute for Cancer Research, the Cancer Stem Cell Consortium via Genome Canada and the Ontario Genomics Institute, the Canadian Institutes of Health Research, the Canadian Cancer Society, the Terry Fox Foundation, a Canada Research Chair and The Princess Margaret Cancer Foundation.
Read the full news release: http://www.uhn.ca/corporate/News/PressReleases/Pages/stem-cell_researchers_solve_mystery_relapse_acute_myeloid_leukemia.aspx
Read the paper: http://www.nature.com/nature/journal/vaop/ncurrent/full/nature22993.html